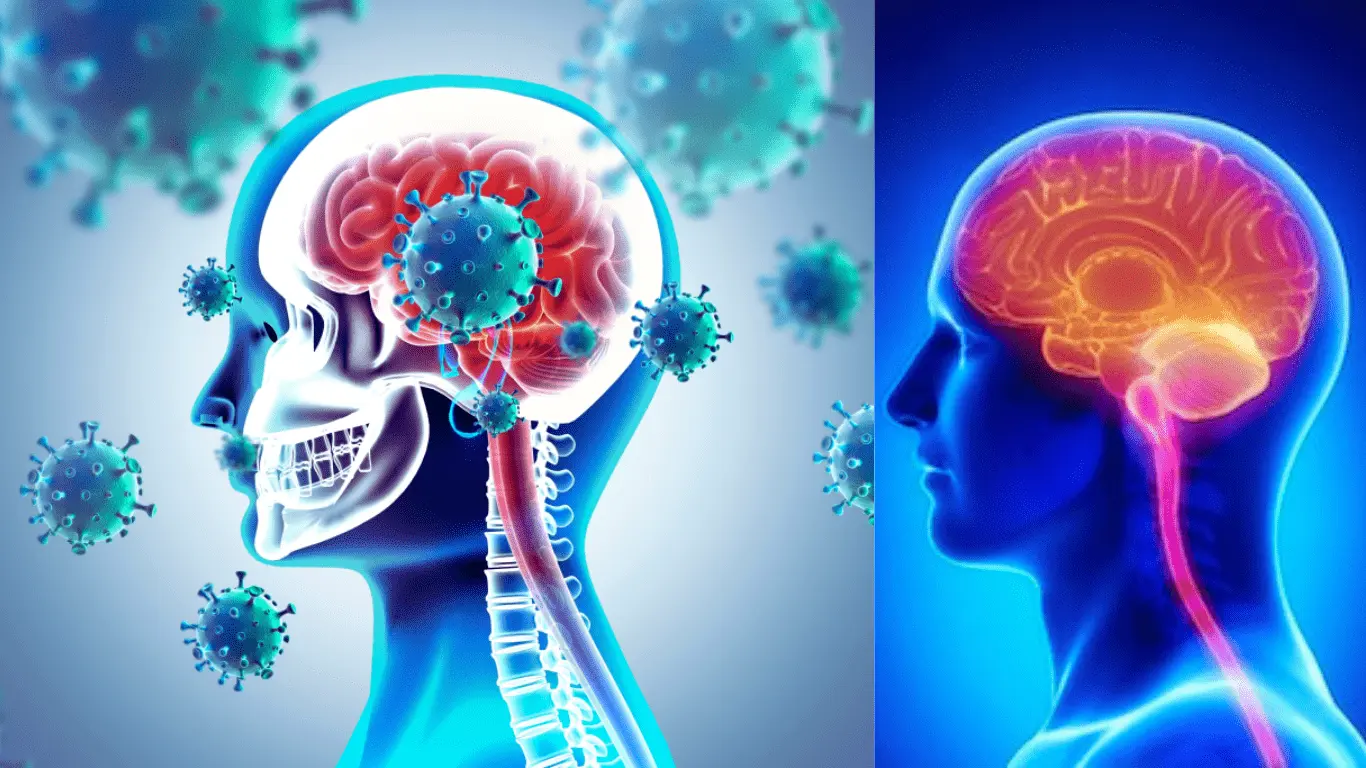
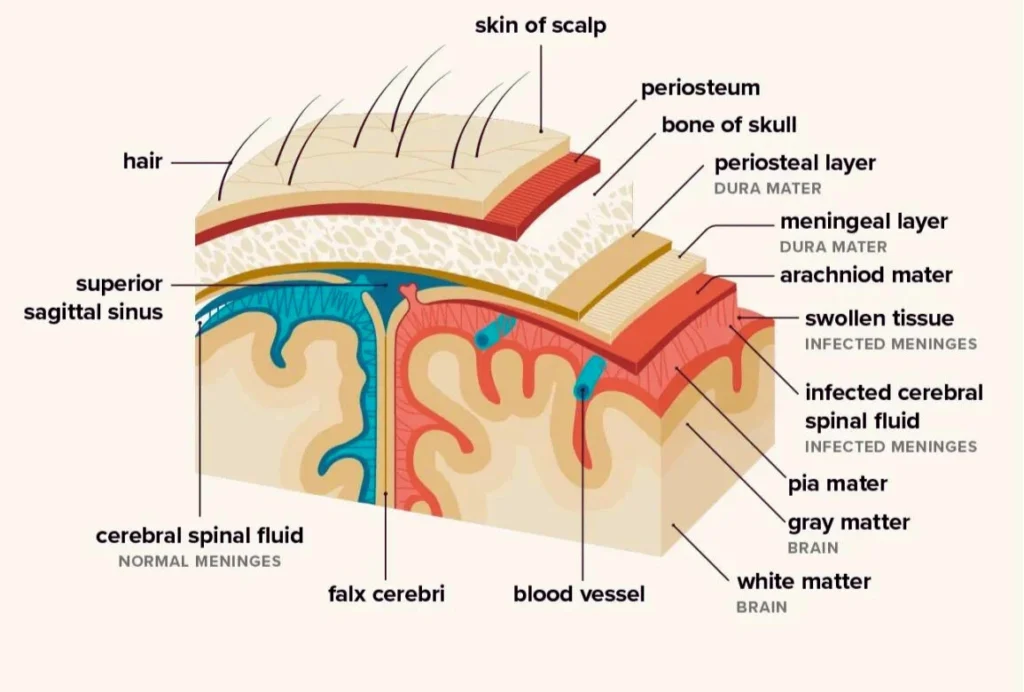
Meningitis is an inflammation of the meninges, the protective membranes covering the brain and spinal cord, and often involves the fluid-filled space around these areas. It can be caused by bacteria, viruses, and less commonly by fungi or parasites. This condition is considered life-threatening, especially when caused by bacteria, as it can lead to severe health complications and requires immediate medical attention. The disease can manifest symptoms such as headaches, fever, and a stiff neck. Diagnosis typically involves methods like lumbar punctures (spinal taps) to examine the cerebrospinal fluid. Meningitis is a major public health challenge due to its potential to cause widespread outbreaks, particularly those caused by the bacteria Neisseria meningitidis.
Types of Meningitis
Viral Meningitis

Viral meningitis is the most common form of meningitis and is generally less severe than bacterial meningitis. It involves the inflammation of the meninges, which are the protective membranes covering the brain and spinal cord, due to a viral infection.
Common symptoms include headache, stiff neck, fever, nausea, and vomiting. Although the disease is often less severe, it can still have long-lasting effects and significantly impact quality of life.
Enteroviruses, particularly the Coxsackie and Echovirus groups, are the most frequent viral causes of meningitis. These viruses are usually transmitted through fecal contamination or respiratory droplets. Most cases of viral meningitis are self-limiting, and patients generally recover without specific antiviral treatment.
Bacterial Meningitis
Bacterial meningitis is a severe, potentially life-threatening infection that causes inflammation of the meninges, the protective membranes covering the brain and spinal cord. This type of meningitis is serious, with the possibility of death occurring within a few hours of symptom onset.
The primary bacteria responsible for bacterial meningitis include Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), and Haemophilus influenzae. These bacteria are commonly carried in the human nose and throat, and can occasionally breach the body’s defenses and infect the meninges.
Fungal Meningitis
Fungal meningitis is a rare and typically non-contagious form of meningitis, which is an inflammation of the membranes (meninges) covering the brain and spinal cord. It is caused by a fungal infection and can develop when fungus spreads from a source elsewhere in the body to the brain or spinal cord or is introduced directly into the central nervous system. Common fungi responsible for meningitis include Cryptococcus, Histoplasma, Blastomyces, Coccidioides, and Candida.
The infection often develops gradually, presenting symptoms such as persistent headaches, low-grade fever, nausea, confusion, and sensitivity to light over weeks. Due to the nonspecific nature of its symptoms and slower onset, diagnosis can be challenging.
Fungal meningitis is typically seen in individuals with weakened immune systems, such as those with AIDS, cancer, or other conditions that impair immune function.
Parasitic Meningitis

Parasitic meningitis, also known as eosinophilic meningitis, is a rare form of meningitis caused by the infection of the protective membranes (meninges) surrounding the brain and spinal cord by parasites. This type of meningitis is not spread from person to person but can be contracted by ingesting parasites, which are often found in soil, water, feces, some animals, or consuming raw or undercooked foods.
One specific cause of parasitic meningitis is Naegleria fowleri ameba, which leads to a condition called Primary Amebic Meningoencephalitis (PAM). This typically occurs when water containing the ameba enters the body through the nose, as in swimming in warm freshwater bodies.
Another parasite known to cause this condition is Angiostrongylus cantonensis, which can lead to human parasitic meningitis, particularly prevalent in Taiwan. This typically happens when individuals consume raw or undercooked snails carrying the parasite.
Causes and Risk Factors
Causes
Meningitis can be triggered by a variety of factors, primarily by infections but also by other conditions:
1. Viral Meningitis:
This is the most common and generally the least severe form of meningitis. It is usually caused by enteroviruses, but other viruses such as the mumps virus, HIV, and herpes viruses can also cause viral meningitis.
2. Bacterial Meningitis:
More serious than viral meningitis, it can be caused by several types of bacteria:
- Neisseria meningitidis (meningococcus) commonly leads to bacterial meningitis in adolescents and young adults.
- Streptococcus pneumoniae, which is the leading cause of bacterial meningitis in infants, young children, and adults in the United States.
- Group B Streptococcus, particularly in newborns, is sourced from the maternal genital tract.
- Haemophilus influenzae type b (Hib) was once the leading cause of bacterial meningitis in children but has become less common due to vaccination.
3. Fungal Meningitis:
This less common form of meningitis is usually caused by the spread of a fungus through blood to the spinal cord. Commonly, cryptococcal meningitis is seen in people with suppressed immune systems, such as those with AIDS.
4. Non-infectious Meningitis:
Caused by diseases, medical treatments, or injuries:
- Chemical reactions, drug allergies, and inflammatory diseases like sarcoidosis can lead to aseptic meningitis.
- Cancer, certain drugs, and other types of infections can also be underlying causes of non-infectious meningitis.
Risk Factors
Common risk factors for meningitis, particularly bacterial meningitis, include:
- Age: Infants are at higher risk due to their still-developing immune systems.
- Compromised Immune System: Individuals with weakened immune systems from conditions such as HIV/AIDS, diabetes, or taking immunosuppressive medications are more susceptible.
- Community Living: Living in communal settings, such as college dormitories or military barracks, increases the risk due to close contact with others.
- Travel: Travel to or residing in parts of the world where meningitis is more common can increase risk.
- Previous Infections: Having a respiratory infection or a cold can increase susceptibility to meningitis.
- Medical History: Certain medical procedures or conditions that impact the head or immune system can also increase risk.
These factors can significantly contribute to the likelihood of developing meningitis, underscoring the importance of preventive measures and awareness.
Symptoms of Meningitis
Early Symptoms
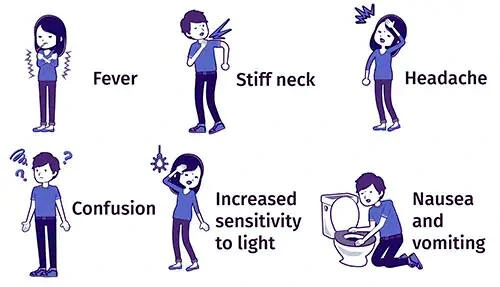
The early symptoms of meningitis can appear quickly and are critical to recognize promptly. These initial signs include:
- Fever: A sudden high fever is often one of the first signs.
- Severe Headache: This is not a typical headache and is often described as ‘severe’.
- Neck Stiffness: Difficulty bending the neck and extreme discomfort are common.
- Nausea and Vomiting: These symptoms can accompany the headache and fever.
- Confusion and Reduced Alertness: Individuals may appear less lucid, and their attention span may be diminished.
- Sensitivity to Light: Photophobia, or sensitivity to light, is also frequently reported.
- Other flu-like symptoms: These might precede more specific signs, including muscle pain, cold hands and feet, or lethargy.
Recognizing these symptoms early can be crucial for effective treatment and can significantly impact the prognosis.
Advanced Symptoms
As meningitis progresses, symptoms can become more severe and lead to serious complications. Advanced symptoms and complications include:
- Seizures: This can occur due to increased pressure and inflammation in the brain.
- Mental status changes: These may include confusion or an inability to concentrate, and in severe cases, can progress to delirium or coma.
- Inability to lower the chin to the chest: This severe neck stiffness can be a sign of substantial irritation and inflammation of the meninges.
- Sensitivity to light (Photophobia): This symptom can increase as the condition worsens.
- Chronic symptoms: These can persist and include headaches and confusion, particularly in chronic meningitis.
Complications from meningitis can be severe and long-lasting, including:
- Hearing loss
- Loss of limbs due to tissue damage from sepsis
- Memory or concentration problems which may persist after recovery.
These complications underscore the importance of early diagnosis and treatment.
Diagnosis and Treatment
Diagnosis Methods

Diagnosing meningitis involves several key tests and methods to identify the presence and cause of the inflammation:
- Lumbar Puncture (Spinal Tap): The definitive test for meningitis. It involves collecting cerebrospinal fluid (CSF) to analyze for white blood cell count, protein levels, and glucose levels compared to blood glucose.
- Blood Tests: These can identify markers of inflammation and the specific pathogens responsible for the infection.
- Nucleic Acid Amplification Tests (NAATs): Techniques like polymerase chain reaction (PCR) are used to quickly identify bacterial DNA in the CSF, providing rapid and accurate results.
- Fungal Detection Tests: Special tests to detect fungal infections, which are crucial in diagnosing fungal meningitis.
These methods are essential for a timely diagnosis to initiate the appropriate treatment regimen.
Treatment Options
The treatment of meningitis varies depending on the causative agent, but it generally includes the following key interventions:
- Bacterial Meningitis: Immediate treatment with intravenous antibiotics is crucial. Corticosteroids may also be administered to reduce inflammation and improve outcomes.
- Fungal Meningitis: For meningitis caused by fungi such as Coccidioides immitis, oral fluconazole is the preferred treatment. Dosing typically starts at 400 mg per day, and adjustments may be made based on clinical response.
- Supportive Care: Supportive treatments for meningococcal disease may include breathing support, medications to stabilize blood pressure, surgery to remove dead tissue, and intensive wound care for any damaged skin areas.
- Alternative Antibiotics: If standard treatments are not suitable, alternatives like chloramphenicol can be used against both gram-negative and gram-positive bacteria, including in cases of meningococcal infection.
These treatments aim to quickly manage the infection and prevent serious complications or death.
Prevention and Vaccines
Preventive Measures
To prevent the spread of meningitis, especially bacterial meningitis, several safety practices and hygiene measures are recommended:
- Vaccination: Vaccines are highly effective in preventing various types of bacterial meningitis. Regular vaccinations are recommended to protect against diseases like meningococcus.
- Personal Hygiene: Frequent and thorough hand washing with soap and water or using an alcohol-based hand sanitizer is crucial to reduce the risk of infection.
- Avoid Sharing Personal Items: Do not share eating utensils, water bottles, glasses, or other items that come into contact with the mouth. This practice helps prevent the transmission of the disease.
- Maintain Clean and Safe Interactions: Avoid close contact such as kissing, hugging, or any other activity that involves close physical contact with others, especially if they are showing symptoms of illness.
- Droplet Precautions: Be aware of the importance of containing sneezes and coughs to prevent the spreading of infectious droplets in environments like schools and workplaces.
These preventive measures can significantly reduce the risk of contracting and spreading meningitis.
Role of Vaccines
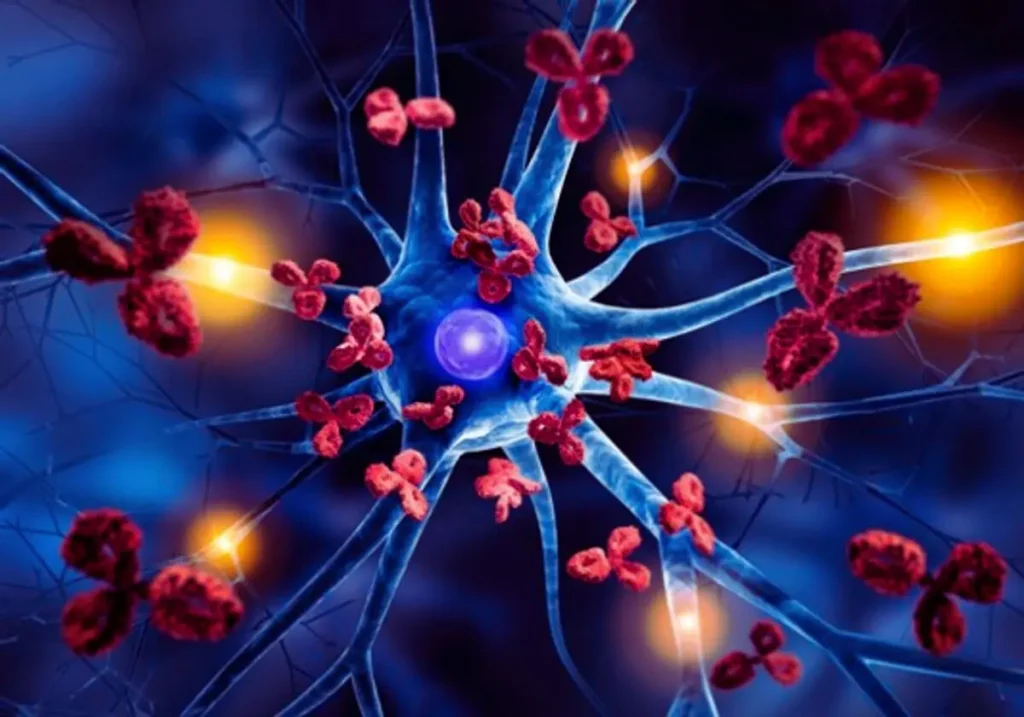
Vaccines play a crucial role in preventing meningitis, particularly meningococcal disease, by preparing the immune system to recognize and fight the bacteria that cause this serious condition:
- Introduction of Antigens: Meningitis vaccines work by introducing small, harmless pieces of the bacteria (antigens) into the body, prompting the immune system to respond. This response helps the body develop protective antibodies without causing the disease.
- Protection Against Specific Strains: Specific vaccines like Bexsero® are designed to protect against particular serogroups of meningococcal disease, such as serogroup B.
- Reduction of Carriers: Vaccination not only protects the individual from getting sick but also reduces the number of people who carry the bacteria in their nose and throat, thereby decreasing the spread of the disease to others.
- Creation of Immunological Memory: The immune system remembers the encounter with the antigens introduced by the vaccine, enabling a quicker and more effective response to future exposures to the disease.
These mechanisms make vaccination one of the most effective ways to prevent meningococcal disease and its severe outcomes, including meningitis.
Living with Meningitis
Living with and managing meningitis involves several critical care strategies to address both the acute symptoms and the long-term consequences of the disease:
- Immediate Medical Care: Prompt administration of antibiotics is crucial for bacterial meningitis. Patients often require hospitalization to receive intensive support including intravenous fluids and, if necessary, medications to control seizures and manage pain.
- Airway and Oxygenation: Managing the airway and ensuring sufficient oxygenation are fundamental, especially in severe cases where respiratory support might be needed.
- Fever Management: Controlling fever is a key aspect of care, which can help alleviate some symptoms and prevent further complications.
- Hygiene Practices: Frequent hand washing and avoiding close contact with sick individuals can help prevent the spread of meningitis.
- Follow-up Care: Long-term effects of meningitis such as hearing loss, cognitive deficits, and coordination problems may require ongoing rehabilitation and regular medical follow-ups to monitor and manage these issues effectively.
These strategies are designed to manage symptoms and prevent complications, thereby improving outcomes for those living with meningitis.
Conclusion
Meningitis is intense and potentially life-threatening, but with prompt treatment and preventive measures, outcomes can be significantly improved.
Read also: What is MSG?
FAQs
Q. Can meningitis be cured?
Yes, especially if treated early. The prognosis depends on the meningitis type and the treatment’s promptness.
Q. How fast does meningitis progress?
Symptoms can progress over several hours to a few days, making quick medical response crucial.
Q. Who is most at risk for meningitis?
Infants, teenagers, and people with weakened immune systems are at higher risk.
Q. Are there long-term effects of meningitis?
Some types, especially bacterial, can have long-term effects such as hearing loss or cognitive impairments.
Q. How can I tell if it’s meningitis and not the flu?
The stiff neck, severe headache, and high fever are tell-tale signs, but a medical diagnosis is necessary to be sure.