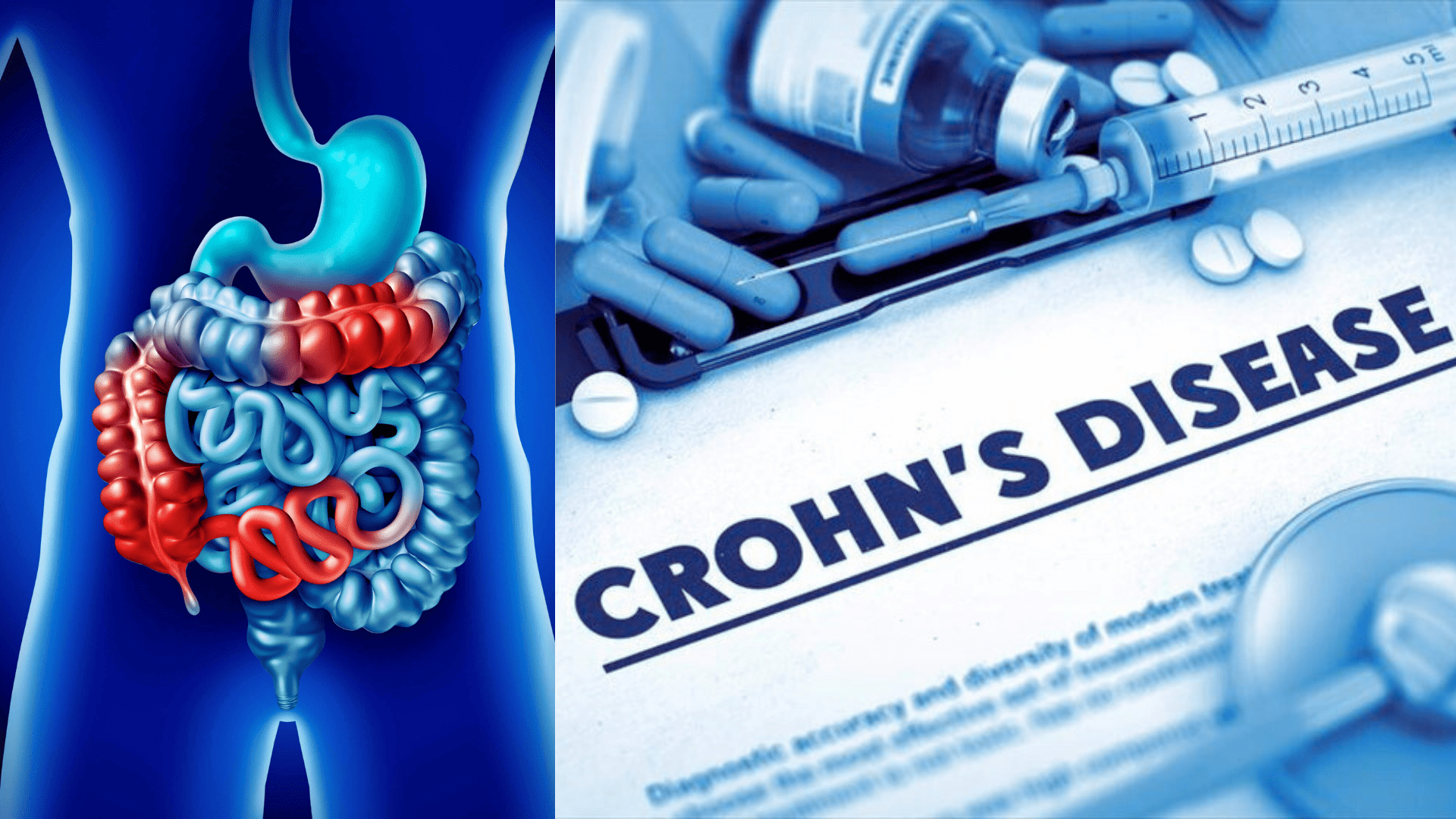
Crohn’s disease is a chronic inflammatory condition classified under inflammatory bowel disease (IBD). It primarily affects the gastrointestinal tract, causing inflammation that can span from the mouth to the anus, though it most commonly targets the end of the small intestine (ileum) and the beginning of the colon. This inflammation can penetrate deep into the layers of the bowel tissue, which can lead to symptoms such as severe diarrhea, abdominal pain, fatigue, weight loss, and malnutrition.
The disease is characterized by periods of flare-ups followed by times of remission. The exact cause of Crohn’s disease is unknown, but it is thought to result from a combination of genetic predispositions and environmental factors that trigger an abnormal immune response to the intestinal microbiota. There is no cure for Crohn’s disease, but treatments are available that can help manage symptoms and improve the quality of life for those affected.
Understanding Crohn’s Disease
Causes of Crohn’s Disease
The exact cause of Crohn’s disease is not fully understood, but it is thought to result from a complex interplay of factors:
- Immune System Response: It is believed that Crohn’s disease may be an immune response gone wrong, where the immune system attacks the gastrointestinal tract, possibly mistaking bacteria, food, and other substances for foreign invaders.
- Genetics: There is a genetic predisposition to Crohn’s disease, as it is more common in people who have family members with the disease. This suggests that genes play a role in increasing susceptibility.
- Environmental Factors: Certain environmental factors such as diet, smoking, and possibly stress are also thought to contribute to the development of Crohn’s disease. For instance, smoking is known to be a risk factor that not only contributes to the development but can also exacerbate the disease.
- Gut Microbiota: Alterations in the gut microbiome may also play a crucial role in the pathogenesis of Crohn’s disease. The imbalance in the microbial flora can trigger an inflammatory response in the intestinal wall.
These factors, individually or combined, may contribute to the chronic inflammation observed in Crohn’s disease.
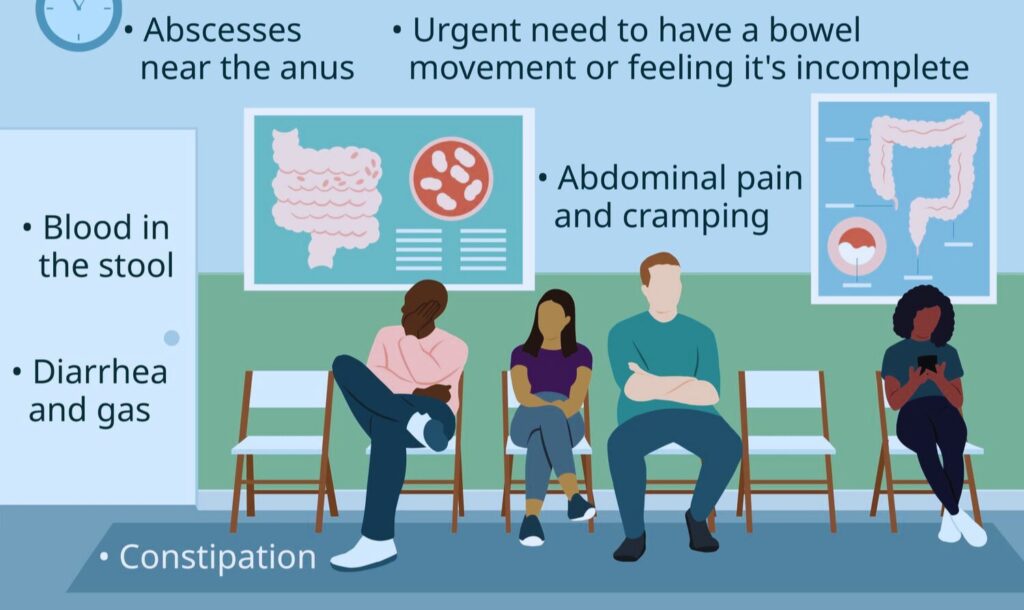
Symptoms
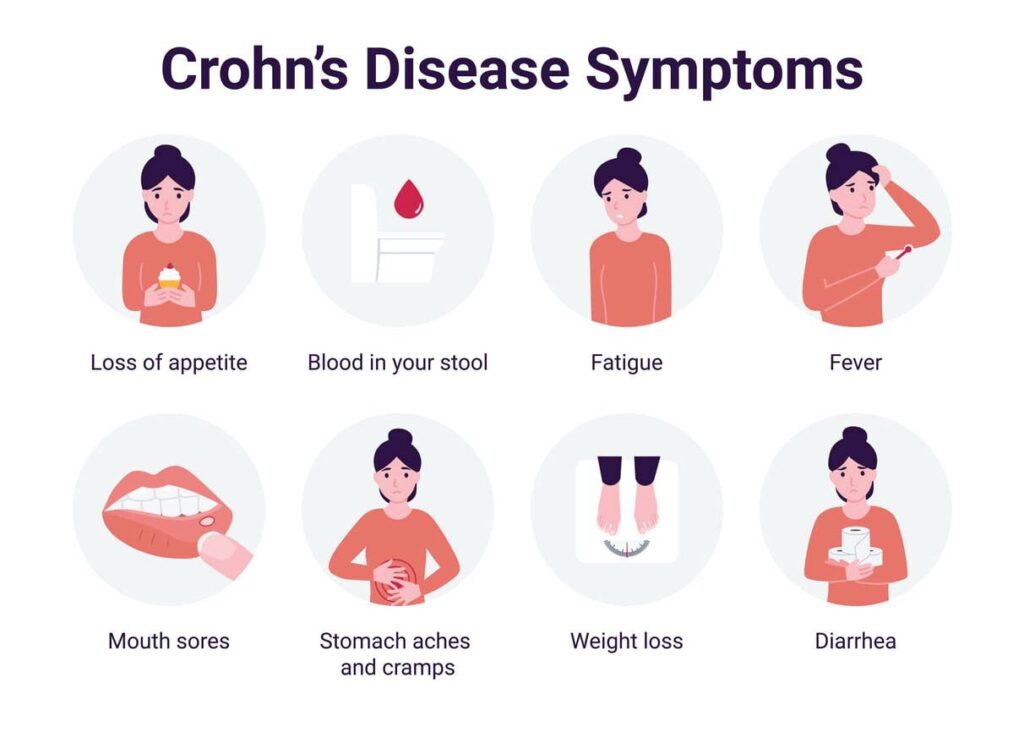
Crohn’s disease symptoms can vary widely but typically involve the gastrointestinal tract. Common symptoms include:
- Abdominal Pain and Cramping: Often the pain is in the lower right abdomen. It can be severe and is usually related to eating.
- Diarrhea: Frequent, uncontrolled diarrhea is a hallmark of Crohn’s, caused by inflammation in the intestines.
- Weight Loss: Involuntary weight loss can occur due to decreased appetite, malabsorption of nutrients, or both.
- Fatigue: Many people with Crohn’s experience a persistent feeling of tiredness, which can be exacerbated by anemia.
- Blood in the Stool: This may appear as bright red blood or darker tar-like stool, indicating bleeding in the GI tract.
- Fever: During active flare-ups, fevers may occur, reflecting inflammation or infection.
- Mouth Sores: Can appear during periods of immune activity related to Crohn’s.
- Perianal Disease: Pain or drainage near or around the anus due to inflammation from a fistula or abscess.
Diagnosis
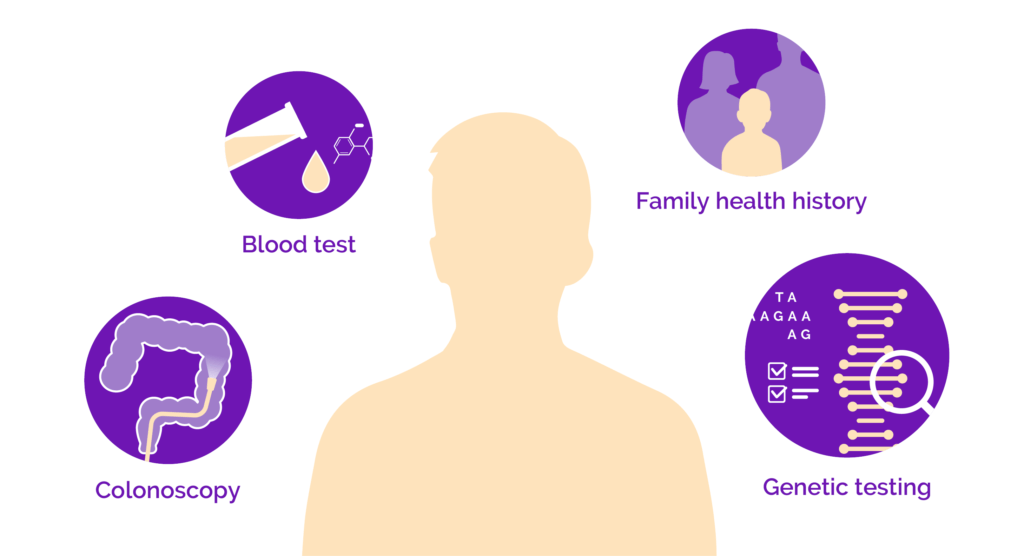
Diagnosing Crohn’s disease involves a combination of tests and procedures to distinguish it from other gastrointestinal conditions and confirm the presence of inflammation and tissue damage. Common diagnostic methods include:
- Blood Tests: These are used to check for signs of inflammation through elevated C-reactive protein (CRP) levels or anemia.
- Endoscopic Procedures: Intestinal endoscopies, such as a colonoscopy, allow direct visualization of the bowel’s condition to assess inflammation and take tissue biopsies for histological examination.
- Imaging Tests: Techniques such as CT scans, MRI, and X-rays are used to view the gastrointestinal tract, detect complications, and assess the extent of the disease beyond what can be seen via endoscopy.
- Stool Tests: These help in ruling out infections that might mimic Crohn’s symptoms, such as parasitic, viral, or bacterial pathogens.
- Antibody Tests: Tests for specific antibodies like anti-Saccharomyces cerevisiae (ASCA) and perinuclear anti-neutrophil cytoplasmic antibodies (pANCA) can support a diagnosis of Crohn’s disease.
Living with Crohn’s Disease
Treatment Options

The treatment of Crohn’s disease involves various strategies aimed at reducing inflammation, maintaining remission, and managing symptoms. Here are some of the key treatment approaches:
- Medication: The use of anti-inflammatory drugs like corticosteroids and immune system suppressors is common. Medications like 6-methylprednisolone have shown high efficacy in managing Crohn’s disease symptoms.
- Biologic Therapies: Anti-TNF agents and other biologics targeting specific components of the immune system can be very effective, especially in severe cases. Combination therapy involving anti-TNF and thiopurines is a particularly effective strategy for moderate to severe Crohn’s disease.
- Antibiotics: These can be effective in addressing complications that arise from bacterial overgrowth or infections secondary to Crohn’s disease. Their usage varies among patients and scenarios.
- Surgery: While not a cure, surgery may be necessary to deal with complications like strictures, fistulas, or severe diseases that do not respond to other treatments. Nearly half of all Crohn’s disease patients might require surgical intervention at some point.
These treatments vary in their effectiveness and are often tailored to individual patient needs, depending on the severity and location of their disease.
Diet and Nutrition

Dietary management for Crohn’s Disease includes several strategies aimed at reducing symptoms and promoting intestinal healing:
- Low Red and Processed Meat Consumption: While a diet low in red and processed meats may help reduce flare-ups in ulcerative colitis, it has not shown the same efficacy in Crohn’s disease for reducing relapses.
- High Fiber from Plants: A high fiber intake, especially from plant sources like fruits, vegetables, grains, beans, and nuts, is generally recommended unless during a flare-up or in cases with strictures where a low residue diet might be necessary.
- Low-Residue Diet: During flare-ups, following a low-residue diet can help relieve symptoms like abdominal pain and diarrhea. This diet limits high-fiber foods, which can decrease bowel volume and reduce discomfort.
- Exclusive Enteral Nutrition (EEN): EEN involves consuming a liquid formula as the sole source of nutrition for a period, which has been shown to improve disease activity and reduce inflammation markers like C-reactive protein in Crohn’s disease.
Patients with Crohn’s disease must work closely with healthcare providers to tailor dietary approaches based on their specific needs and disease state.
Managing Symptoms
Managing symptoms of Crohn’s Disease effectively involves a combination of dietary adjustments, stress management, and regular communication with healthcare providers:
- Balanced Nutrition: Ensure a balanced intake of proteins, calories, and nutrients to help manage symptoms. Tailor your diet to suit periods of flares or remission and consider working with a nutritionist familiar with inflammatory bowel diseases.
- Stress Management: Since stress can exacerbate Crohn’s symptoms, learning and practicing stress management techniques such as exercise, meditation, or other relaxation methods can be beneficial.
- Regular Medical Consultation: Work closely with your gastroenterologist to monitor the disease’s progression and adjust treatment plans as necessary. This includes medication management, routine check-ups, and possibly surgery.
- Low-Residue Diet: During flare-ups, a low-residue diet may help reduce abdominal pain and diarrhea by limiting high-fiber foods.
The Emotional Impact
Crohn’s disease not only affects physical health but significantly impacts mental health, leading to a higher prevalence of anxiety, depression, and other psychological issues:
- Link Between Crohn’s and Mental Health: Individuals with Crohn’s are more likely to experience mental health challenges such as anxiety and depression due to the chronic nature of the disease and its symptoms.
- Psychological Factors: Patients often face feelings of shame, isolation, and body dissatisfaction, which can severely compromise their mental well-being.
- Pediatric Concerns: Younger patients with IBD, including Crohn’s, can experience heightened psychological difficulties, impacting family dynamics and their sense of normalcy.
- Management Strategies: Addressing these emotional effects involves psycho-social support, mindfulness practices, and sometimes professional mental health care. Programs and resources dedicated to mental health and wellness are crucial for managing these aspects.
Research and Innovations
Latest Research
Recent studies and trials have provided new insights and promising approaches in the management and understanding of Crohn’s Disease:
- Stem Cell-Based Therapies: UC Davis Health is leading a study on a promising stem cell-based therapy aimed at offering new treatment avenues for Crohn’s disease patients.
- Treatment Approaches: Research indicates that treating Crohn’s disease more aggressively and earlier in its course can significantly improve patient outcomes.
- New Medications: Clinical trials at UCSD are exploring the efficacy, safety, and tolerability of oral etrasimod, a new medication option for Crohn’s disease, which is currently in Phase 2/3 of testing.
- Challenges in Pediatric Cases: Despite advances, many children with ileal Crohn’s Disease still progress to conditions requiring surgical interventions, highlighting an ongoing challenge in pediatric treatment.
These studies contribute to a deeper understanding and potentially more effective management strategies for Crohn’s Disease.
Future Prospects
Emerging treatments and therapies for Crohn’s Disease focus on enhancing efficacy, and safety, and targeting specific pathways involved in the disease’s pathogenesis:
- Monoclonal Antibodies: Recent advancements include drugs like vedolizumab, a gut-selective monoclonal anti-integrin antibody, and ustekinumab, which targets IL-12 and IL-23. These therapies offer targeted interventions that minimize systemic side effects while addressing the inflammatory processes specific to Crohn’s Disease.
- Advanced Therapy Early in Treatment: A shift in treatment strategy involves providing advanced therapy early in the disease course. This approach aims to control symptoms more effectively and potentially alter the disease trajectory, which could lead to improved long-term outcomes.
- Safety and Efficacy in Emerging Therapies: Despite transformative treatments, the ongoing challenges include balancing treatment efficacy with potential adverse events. This remains a critical aspect in developing new therapies for Crohn’s Disease.
These developments suggest a hopeful outlook for Crohn’s Disease management, emphasizing personalized treatment plans and improved quality of life for patients.
Real Stories
Case Studies
Personal stories from individuals living with Crohn’s Disease highlight the diverse and often challenging experiences faced by patients. Here are a few examples:
- Ellie’s Experience: Ellie’s symptoms started with abdominal pain, mouth ulcers, perianal abscesses, fatigue, and weight loss. She describes the difficulties of growing up with Crohn’s, dealing with both physical symptoms and the emotional impact of the disease.
- Josephine’s Determination: At 16, Josephine has not allowed Crohn’s disease to control her life or deter her from pursuing her dream of playing Division 1 field hockey in college.
- Rachel’s Journey: Rachel shares her ongoing journey with Crohn’s, providing insights into her day-to-day life and how she manages her condition.
These stories reflect not just the hardships of living with Crohn’s Disease but also the resilience and courage of those affected. They serve as valuable resources for understanding the personal impact of the disease beyond medical descriptions.
Conclusion
Crohn’s Disease is a complex, chronic inflammatory bowel disease characterized by a relapsing and remitting course that can progressively worsen over time. Although the exact cause is unknown, it is generally accepted that genetic, environmental, and immunological factors contribute to its development. Treatment strategies have evolved significantly, with anti-TNF therapies making substantial impacts on disease control and patient quality of life. Furthermore, the Crohn’s Disease Exclusion Diet (CDED) has emerged as an effective dietary approach, especially in pediatric and adult cases, providing an alternative to traditional exclusive enteral nutrition (EEN).
Advancements in treatment and management options continue to improve, driven by ongoing research and clinical trials that refine and enhance therapeutic approaches, such as the exploration of biomarkers and treatment strategies in randomized controlled trials. With these evolving therapies, there is hope for more personalized and effective management of Crohn’s Disease in the future.
Read also: What is BlueChew?
FAQs
Q. What is Crohn’s Disease?
Crohn’s disease is a chronic inflammatory condition of the gastrointestinal tract, causing a range of symptoms such as abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition.
Q. Is there a cure for Crohn’s Disease?
Currently, there is no cure for Crohn’s disease. However, there are various treatments available that can greatly reduce the symptoms and even bring about long-term remission.
Q. What are the treatment options?
Treatment for Crohn’s disease usually involves either medication, surgery, or a combination of both. The goal is to reduce inflammation, manage symptoms, and maintain remission.
Q. How challenging is it to live with Crohn’s Disease?
Living with Crohn’s disease can be physically and emotionally challenging. Patients may experience periods of severe symptoms followed by periods of remission. Ongoing medical care is crucial and adapting lifestyle and diet can also help manage the condition.