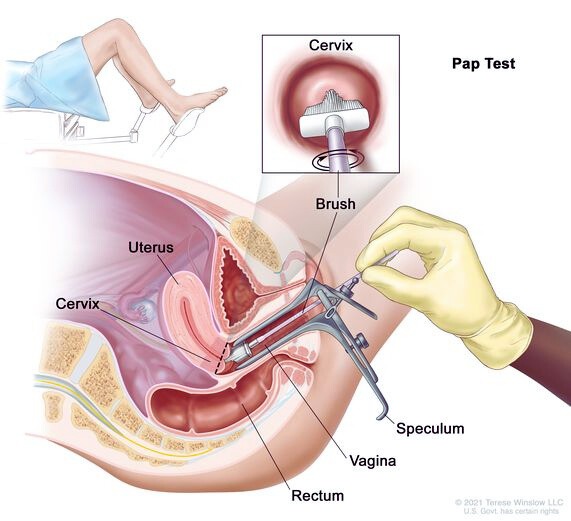
A Pap smear, also known as a Pap test, is a medical procedure used to screen for cervical cancer in women. The test involves collecting cells from the cervix, which is the lower part of the uterus opening into the vagina. These cells are then examined under a microscope to identify any abnormalities that could indicate the presence of precancerous or cancerous conditions.
The significance of a Pap smear lies in its ability to detect cervical changes and conditions early, including infections and inflammation. This early detection is crucial because it can lead to timely intervention, significantly improving the prognosis. The conventional technique for performing a Pap smear involves using a brush and spatula to collect cells from the cervix’s transformation zone, which are then transferred to a slide for examination. Regular Pap smears are recommended for women as part of routine health screenings to monitor and maintain cervical health.
The History of the Pap Smear
Who Invented It?
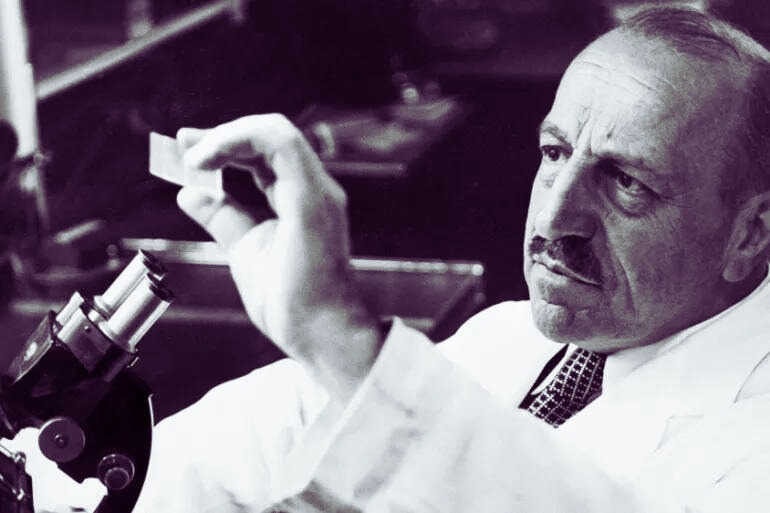
The Pap smear, an essential cervical cancer screening test, was invented by Dr. Georgios Papanikolaou. Dr. Papanikolaou, a Greek physician, developed the test that bears his name, and it has become one of the most successful methods for early detection of cervical cancer. His invention of the Pap smear test in the mid-20th century represented a monumental advancement in women’s healthcare, significantly improving the ability to identify precancerous conditions and cancerous changes in cervical cells at an early stage.
Evolution of the Pap Smear
The Pap smear, developed by Dr. George Papanicolaou in 1928, has significantly evolved as a vital cervical cancer screening tool. Initially reported in 1928, its efficacy was established by 1941. This test revolutionized the early detection of cervical cancer by identifying abnormal cells in the cervix. In the 1940s, the introduction of the Pap Smear marked a turning point when cervical cancer was a leading cause of death among women.
Over the decades, the Pap smear has undergone several changes to improve its accuracy and implementation. The test was adopted gradually, as the field of cytopathology developed, and confidence in its effectiveness grew, notably in countries like Canada. Today, due to widespread cervical cancer screening with the Pap smear, cervical cancer is relatively rare in many parts of the world, such as the United States.
Why is a Pap Smear Important?
Cancer Screening
A Pap smear is crucial for cervical cancer screening because it can detect abnormal cells in the cervix before they develop into cancer. Early detection through a Pap smear significantly reduces the risk of developing cervical cancer and decreases cervical cancer-related death rates. The test searches for precancerous or cancerous cells on the cervix, which, if found early and treated appropriately, can prevent the development of cervical cancer.
Who Needs a Pap Smear?
Recommended Age and Frequency
Pap smears, a key screening tool for cervical cancer, are recommended for women based on their age and risk factors. The guidelines for Pap smear screening are as follows:
- Women aged 21-29: Should undergo a Pap smear every 3 years. HPV testing is not routinely recommended for this age group but can be considered for those aged 25 to 29.
- Women aged 30-65: Should have a Pap smear every 3 years or they can choose to have an HPV test every 5 years, or a combination of Pap test and HPV test every 5 years (co-testing).
Regular screening should begin at age 21 regardless of the commencement of sexual activity. Continued regular screening is crucial as it helps detect any cervical changes early before they potentially develop into cancer.
Risk Factors and Exceptions
Pap smears are generally recommended for women as part of routine cervical cancer screening. However, certain risk factors may necessitate more frequent screenings or screenings for those who might not typically require them:
- Age over 30: HPV infection becomes a significant risk factor for cervical cancer, necessitating routine screening.
- Immunocompromised Individuals: Those with weakened immune systems, including HIV-positive individuals, may need more frequent Pap smears due to higher susceptibility to infections and cancer.
- Previous Cervical Cancer or Precancerous Findings: Individuals who have had cervical cancer or precancerous cervical lesions should follow a more frequent screening schedule, as recommended by their healthcare provider.
Women typically begin Pap smear screenings at 21 and continue until about 65, unless other risk factors or previous medical history indicate otherwise. Beyond the general guidelines, specific circumstances might require adjustments to the screening schedule as determined by healthcare providers.
What Happens During a Pap Smear?
Before the Test
Before a Pap smear test, a few preparatory steps are typically followed:
- Scheduling the Test: The test should be scheduled when a woman is not menstruating, ideally mid-menstrual cycle, as this provides the clearest sample of cervical cells.
- Avoiding Certain Activities: Before the test, it is recommended to avoid intercourse, douching, or using any vaginal medicines or spermicidal foams, creams, or jellies for two days before the test, as these may wash away or obscure abnormal cells.
- During the Appointment: The test involves the insertion of a speculum into the vagina to widen it. This allows the healthcare provider to view the cervix and collect cells from the cervix using a small brush or spatula. The cell sample is then sent to a laboratory for analysis to check for the presence of precancerous or cancerous cells.
The process is quick and usually causes minimal discomfort. It’s important for patients to be relaxed and to breathe normally to ease the insertion of the speculum.
The Procedure Itself
During a Pap smear, the following steps are generally taken:
- Preparation: The patient is asked to undress from the waist down and lie on an exam table with their feet placed in supports called stirrups.
- Speculum Insertion: A healthcare provider inserts a speculum into the vagina. The speculum is a device that holds the vaginal walls apart to allow access to the cervix, the lower part of the uterus that opens into the vagina.
- Collecting the Cells: Using a soft brush or a small spatula, the provider gently scrapes or brushes the surface of the cervix to collect a sample of cervical cells. This procedure is typically quick and may cause some discomfort, like mild cramping or pressure.
- Sample Analysis: The collected cells are then placed on a glass slide or in a liquid vial and sent to a laboratory where they are examined under a microscope to identify any abnormalities that could indicate precancerous changes or cervical cancer.
The procedure is usually done quickly and is a critical part of routine preventive healthcare for women, helping detect early signs of cervical cancer.
After the Test
After a Pap smear test is completed, the following steps occur:
- Sample Processing: The sample of cervical cells collected during the Pap smear is sent to a laboratory. There, it is examined under a microscope by cytotechnologists and pathologists to detect the presence of abnormalities.
- Results Notification: The results are usually ready within a few weeks. The patient will be notified of the results by their healthcare provider. If the test results are normal, no further action is typically required until the next scheduled screening.
- Follow-Up: If abnormal or unclear results are detected, further testing or follow-up may be necessary. This could include a repeat Pap test, a test for human papillomavirus (HPV), or a more detailed examination called a colposcopy to more closely inspect the cervix, vagina, and vulva.
What Do the Results Mean?
Normal Results
Normal results from a Pap smear mean that no abnormal cells were detected on the cervix during the screening. This outcome is often referred to as a “negative” result, indicating that there is no evidence of precancerous or cancerous cells at the time of testing. Patients with normal results typically continue with routine screening at intervals recommended by their healthcare provider, which generally depends on their age, medical history, and risk factors for cervical cancer.
Abnormal Results
Possible Abnormalities
Abnormal results from a Pap smear do not automatically imply the presence of cervical cancer but indicate the detection of abnormal cells on the cervix, which could suggest several possibilities:
- ASC-US: Atypical squamous cells of undetermined significance, where changes in the cells are observed but not indicative of a pre-cancerous condition.
- Dysplasia: Presence of precancerous cells that could potentially develop into cervical cancer if not monitored or treated appropriately.
- HPV Infection: Human papillomavirus infection, a common cause of cervical cancer, might be indicated by an abnormal Pap smear, necessitating further testing.
- Inflammation: Sometimes, inflammation or minor infections can cause cell changes detected by a Pap smear, which may not be serious.
These results usually lead to follow-up tests, including repeat Pap smears, HPV testing, or more detailed examinations like a colposcopy to determine the nature and extent of the abnormalities detected.
Follow-Up Procedures
When a Pap smear yields abnormal results, the follow-up procedures can vary based on the type of abnormality detected, patient age, and medical history:
- Repeat Testing: A second Pap test or an HPV test may be recommended to confirm the initial findings and assess the presence of HPV, which is strongly linked to cervical cancer.
- Colposcopy: This procedure involves a detailed examination of the cervix using a special microscope called a colposcope to identify and examine abnormal areas more closely. It is commonly recommended for high-grade abnormalities (HSIL).
- Reflex Testing: If an HPV test was not done initially with the Pap test, it might be conducted as a follow-up to determine if HPV is present, helping to guide further actions.
- Biopsy: During a colposcopy, a biopsy may be performed where a small piece of tissue is removed from the cervix for closer examination under a microscope to detect precancerous or cancerous cells.
These steps help determine the necessity for treatment and the best course of action to take for patient care.
Common Questions and Myths
Debunking Common Myths
Pap smears are surrounded by myths that can cause unnecessary worry. Here are some common misconceptions debunked:
- Myth: Pap Smears Need to be Done Annually: The recommendation for Pap smears has changed over the years. Most women do not need an annual Pap smear. The frequency depends on your age, medical history, and previous test results.
- Myth: Pap Smears are Painful: While it’s true that a Pap smear can be uncomfortable for some, it is generally not painful. The discomfort, if any, is brief.
- Myth: Screening has No Risks: Screening, including Pap smears, can sometimes lead to over-diagnosis and unnecessary treatments. It’s important to discuss the potential harms and benefits with your healthcare provider.
By clarifying these myths, women can approach Pap smear screenings with more confidence and less anxiety.
The Future of Pap Smears
Technological and Methodological Advances
Recent advancements in the technology and methodology of Pap smears are set to significantly enhance cervical cancer screening. These innovations include:
- Liquid-Based Cytology (LBC): This method offers clearer and more accurate samples by reducing the presence of other materials like blood or mucus, which sometimes obscure cytological examination.
- Human Papillomavirus (HPV) Testing: Integration of HPV testing in cervical screening is a major shift, providing earlier identification of high-risk infections that are likely to lead to cervical cancer.
- Artificial Intelligence (AI) Diagnostics: AI is being explored to analyze Pap smear results with high accuracy, reducing human error and potentially speeding up diagnosis times. This use of AI can help in recognizing subtle patterns that may not be easily noticeable by human eyes.
These advancements aim to improve the detection of cervical cancer at earlier stages, reduce false negatives, and enhance the efficiency of screenings.
Conclusion
A Pap smear is a simple yet powerful test that is a key part of women’s health. Understanding what it involves, why it’s done, and how to interpret the results can empower you to take charge of your health effectively.
Read also: What Causes Restless Leg Syndrome?
FAQs
Q. How often should I get a Pap smear?
Generally, every three years if your past tests were normal. Your doctor might suggest a different schedule based on your health history.
Q. Is a Pap smear painful?
Most women experience little to no pain—just some discomfort or pressure.
Q. Can I get a Pap smear during my period?
It’s best to schedule the test when you’re not menstruating for clearer results.
Q. What should I do after receiving an abnormal Pap test result?
Follow up with your doctor. They may recommend additional tests to determine the cause of the abnormal cells.